These are the signs that he is cr…See moree

In everyday medical practice, clinicians often make small adjustments to a patient’s treatment plan—switching medications, updating dosages, or changing delivery methods. Most of the time, these changes improve symptoms and enhance quality of life. But occasionally, a routine adjustment can uncover something completely unexpected.
This was the case for a 55-year-old woman living with chronic obstructive pulmonary disease (COPD). For years, her condition remained stable on her medications. Then, after switching to a new inhaler, she developed a painful and rare skin condition known as Sweet syndrome—a reaction so unusual that it may represent the first documented case linked to inhaled therapy.
This story highlights why both patients and healthcare providers must remain alert to even subtle changes in the body, especially following medication adjustments.
The Patient’s Journey: From Stability to Sudden Symptoms
The patient’s medical background included hypertension and long-term COPD management. Her treatment plan featured enalapril for blood pressure control and a formoterol-based inhaler for her respiratory condition. For years, she had been doing relatively well.
But as her lung function began to decline, her pulmonologist decided to adjust her regimen, prescribing a new combination inhaler containing indacaterol and glycopyrronium. This was a standard, evidence-based decision, aimed at improving her breathing and slowing disease progression.
Yet just 48 hours after starting the new inhaler, the patient developed alarming symptoms:
-
Painful, bright red patches on her face and neck
-
A mild fever
-
No new cosmetics, dietary changes, or infections
-
Recent sun exposure, but with proper protection
Her sudden skin reaction and fever prompted an urgent dermatology referral.
The Diagnostic Process: Uncovering Sweet Syndrome

One of the greatest challenges in dermatology is distinguishing between conditions that look alike. Rashes, plaques, and erythematous lesions can arise from dozens of causes, from mild allergies to serious autoimmune disorders.
The initial working diagnoses included:
-
Contact dermatitis
-
Lupus erythematosus
-
Urticaria (hives)
Further investigation revealed the true culprit:
-
Blood tests ruled out common infections and autoimmune markers.
-
The new inhaler was discontinued immediately.
-
A skin biopsy was performed, and pathology confirmed Sweet syndrome.
The patient was started on oral corticosteroids, which produced a dramatic improvement within two days. The plaques faded, her fever subsided, and her pain diminished rapidly.
What Exactly Is Sweet Syndrome?
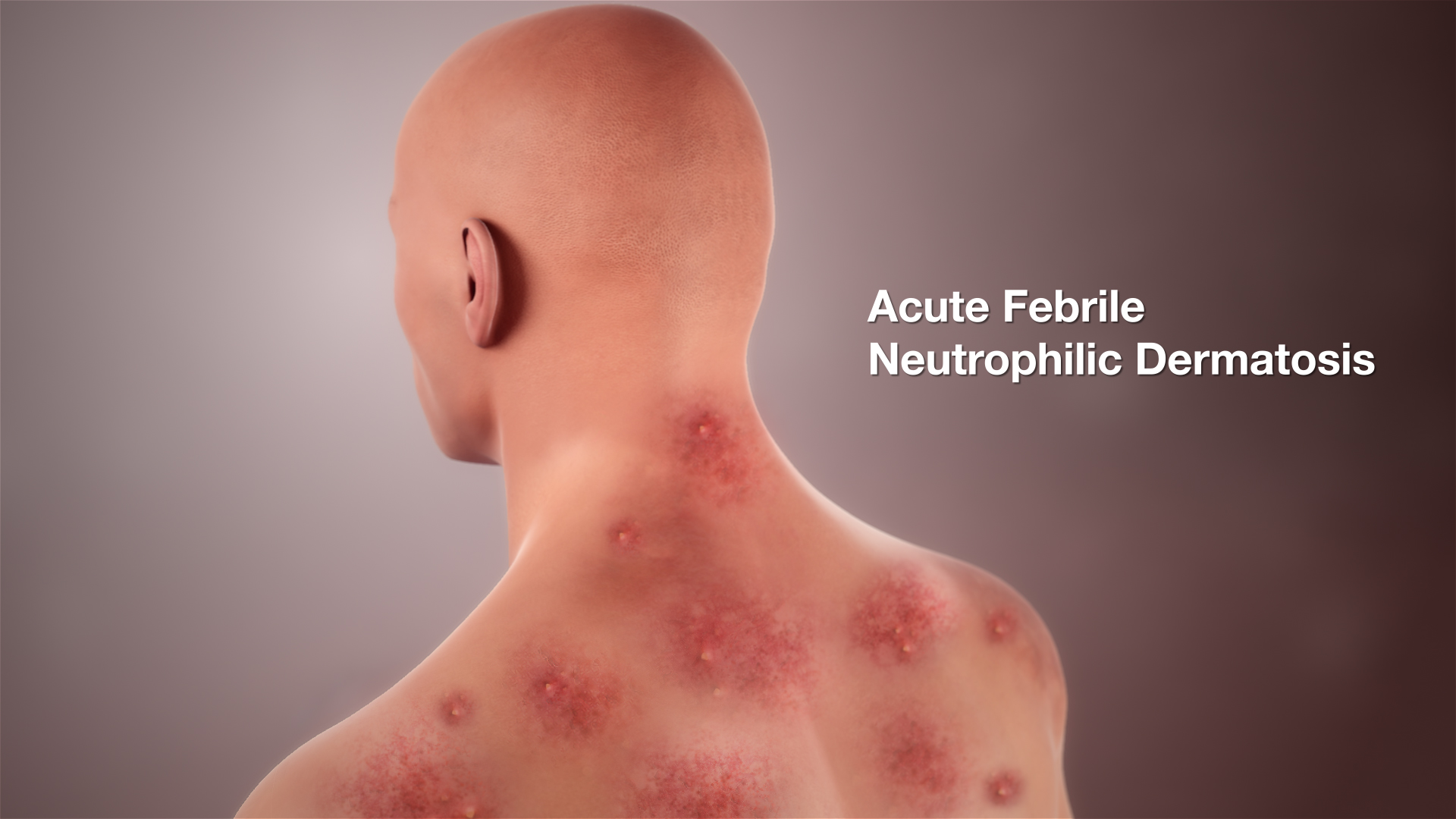
Sweet syndrome, or acute febrile neutrophilic dermatosis, is a rare immune-mediated skin condition first described in 1964 by Dr. Robert Sweet. It is characterized by:
-
Sudden, painful red or purple plaques or papules
-
Lesions concentrated on the face, neck, torso, and hands
-
Accompanying fever, fatigue, and joint pain
-
Elevated white blood cell counts, especially neutrophils
Known Triggers
The exact cause is not fully understood, but it appears linked to immune system dysregulation. Triggers include:
-
Infections (respiratory or gastrointestinal)
-
Hematologic cancers, such as acute myeloid leukemia
-
Autoimmune or inflammatory diseases
-
Medications (antibiotics, antiepileptics, G-CSF, some vaccines)
Treatment typically involves systemic corticosteroids, which usually bring rapid relief.
Why This Case Stands Out

The most striking aspect of this case is that Sweet syndrome was triggered by an inhaled COPD medication. Until now, no cases in medical literature had linked the condition to inhaled therapies.
Clinical Significance
-
Expanding known triggers: Previously, Sweet syndrome was mostly associated with oral or injectable drugs. This case shows even inhaled medications may provoke rare immune responses.
-
Challenges in diagnosis: Because the condition is rare, it can easily be mistaken for more common rashes. Early biopsy is essential.
-
Primary care’s role: General practitioners are often the first to detect unusual reactions. Quick recognition and referral are vital.
Lessons for Clinicians

This case offers several important reminders for healthcare providers:
-
Stay vigilant after medication changes – even widely used drugs can trigger rare immune reactions.
-
Consider Sweet syndrome in sudden, painful skin eruptions with fever.
-
Use a broad differential diagnosis – exclude lupus, dermatitis, and drug eruptions carefully.
-
Act quickly with corticosteroids – they remain the most effective treatment.
-
Report rare cases – documentation expands medical knowledge and helps future clinicians.
Patient Perspective: Living Through a Rare Reaction

For the patient, what began as a standard inhaler switch quickly became a distressing experience. Painful facial lesions were both physically and emotionally overwhelming, affecting self-confidence and social interactions.
Her rapid recovery on corticosteroids was reassuring, but the ordeal highlighted the anxiety patients face when dealing with rare, poorly understood conditions. For those with chronic illnesses like COPD, trust in treatment is critical, making open communication from healthcare providers especially important.
The Broader Implications
This unusual case raises broader questions for research and practice:
-
Could other inhaled therapies carry similar immune-mediated risks?
-
Should monitoring systems track rare skin reactions linked to inhalers?
-
How can primary care doctors and dermatologists collaborate more effectively?
Though rare, awareness is the first step toward prevention and better outcomes.
Conclusion: A Reminder for Vigilance
Sweet syndrome is a rare but significant diagnosis requiring clinical suspicion and swift response. While most cases are linked to infections, cancers, or systemic drugs, this case demonstrates that even inhaled therapies may trigger the condition.
For clinicians, the lesson is clear: no medication is entirely risk-free. For patients, reporting unusual symptoms after treatment changes is crucial.
By recognizing atypical presentations and sharing rare case reports, healthcare providers can improve patient safety, outcomes, and confidence in care.
News in the same category
13 Early Signs of Kidney Failure (You Ignore Daily) | Symptoms of Kidney Failure

A 4-Year-Old Girl Nearly Lost Her Life Due to Diabetes, Parents Cried: “We Spoiled Her Too Much!”

A Cyst on the Foot or Wrist: What You Should Know

7 Things Not to Do Before Taking a Shower to Prevent Stroke – Plus 2 Common Mistakes

10 Warning Signs Your Liver Might Be in Trouble
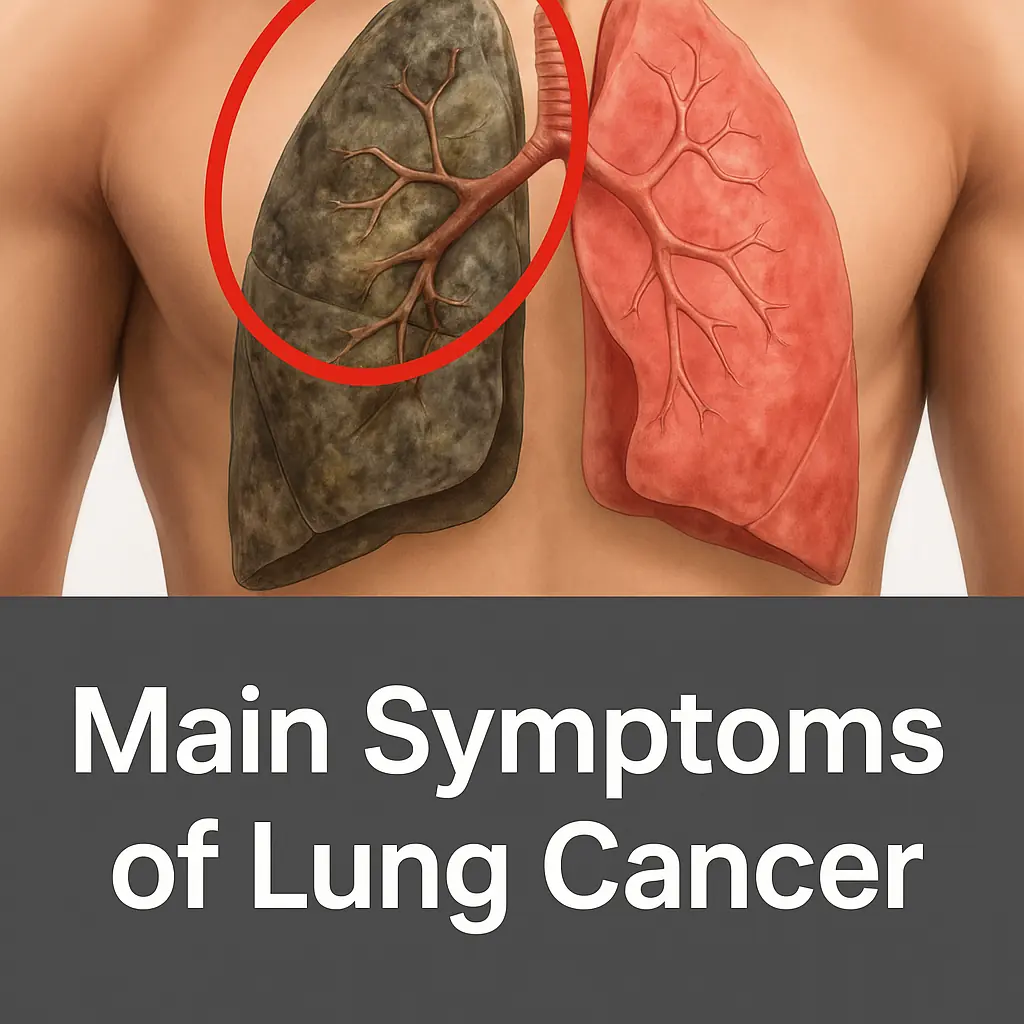
Lung Cancer Symptoms
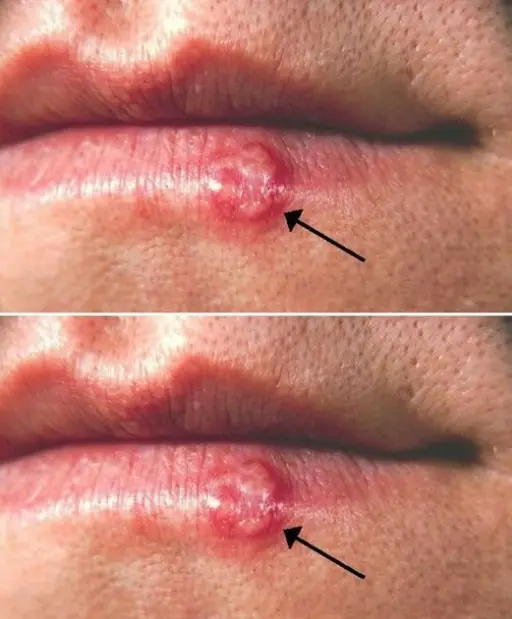
Most People Have Had or Have This Cold Sore Virus, But Very Few Know How to Cure It – Here’s What You Need to Do!

These are the signs that he is cr… See more
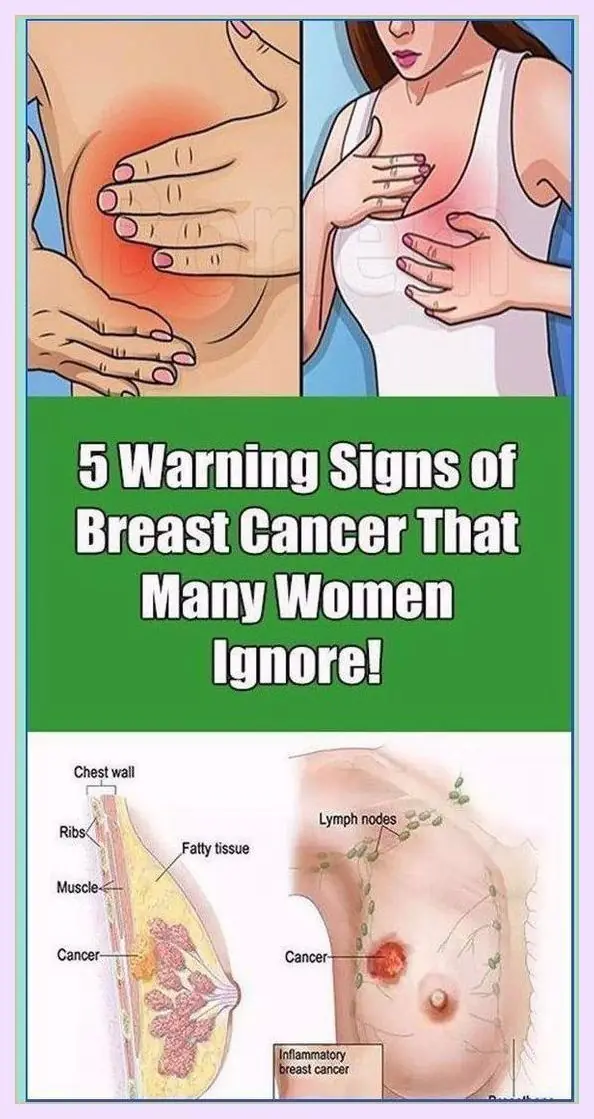
5 Warning Signs of Breast Cancer That Many Women Ignore
Hibiscus Apple Cinnamon Tea with Lemon – A Delicious Detox Drink for Your Health
Everything You Need to Know About Eating Eggs Daily — Science-Backed Benefits & What to Watch For

25 Amazing Ways to Use Rosemary That Can Change Your Life
All DNA and RNA Bases Found in Meteorites: Life’s Origins May Be Cosmic
Doctor reveals the one thing you should avoid doing if you wake up during the night
Claim: a juice regimen reportedly cleared can:cer cells in 42 days

Top 3 Ways to Treat Tooth Decay with Guava Leaves – Simple and Cost-Effective

8 Signs That Your Body Is Crying for Help
News Post
From Foster Care to Fatherhood: One Man’s Mission to Keep Five Siblings Together
15 Deadly Kidney Signs You Must Catch Early
13 Early Signs of Kidney Failure (You Ignore Daily) | Symptoms of Kidney Failure
Japan’s Innovative Parenting Lesson Lets Teens Experience Pregnancy and Infant Care

A New Bird Just Appeared in Texas—and That’s Not a Good Thing

Unlock Garlic’s Hidden Powers: The Ultimate Guide to Transforming Your Health with Nature’s Superfood

Can Okra Water Unlock a Hidden Health Revolution for You? Discover the Secret Elixir
Can Kitchen Staples Unveil a Dazzling Smile in 5 Minutes?

How 15,000 Bikers Rallied in Germany to Fulfill a Dying Boy’s Dream
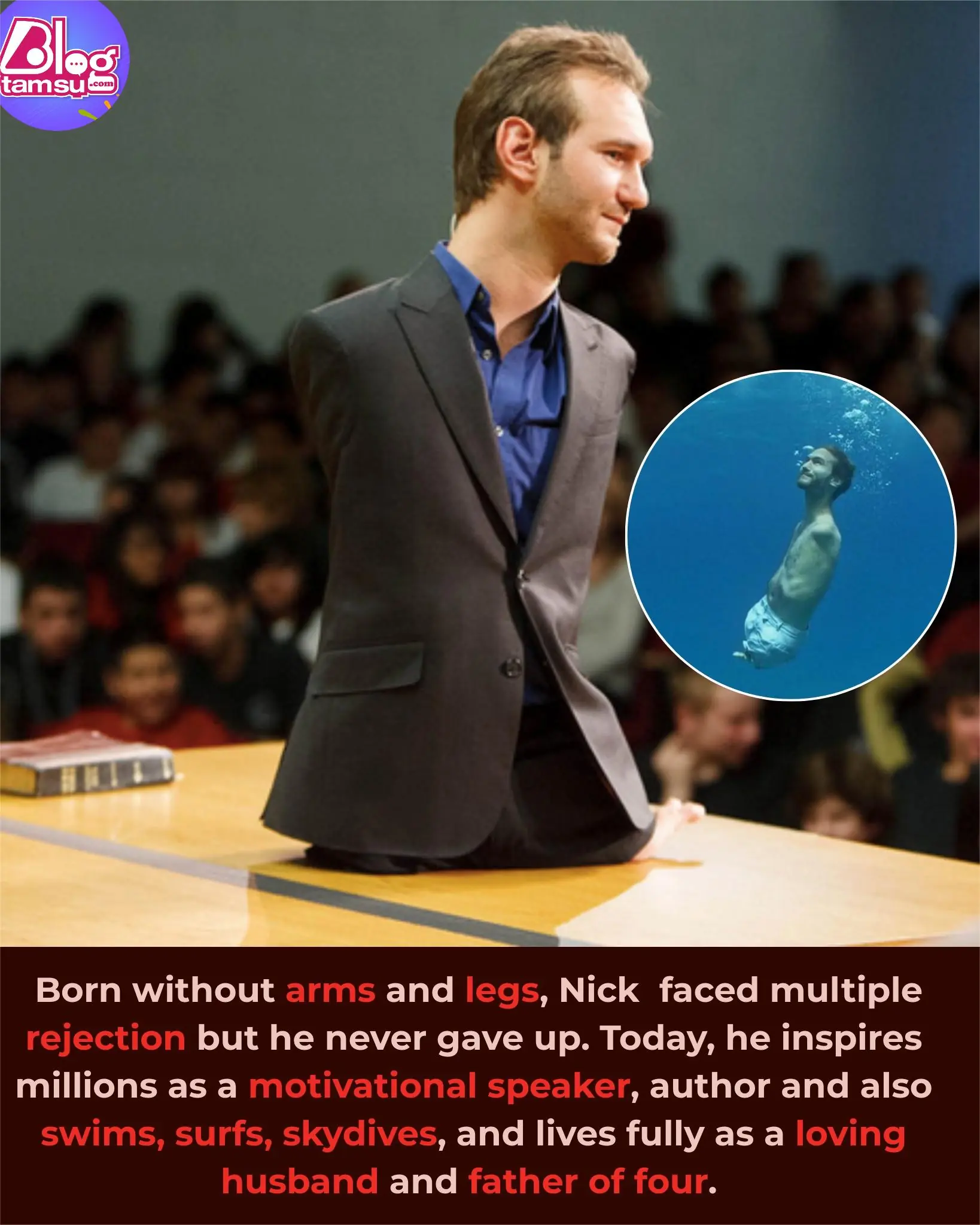
Nick Vujicic: Living Without Limbs, Inspiring Millions Worldwide

Grandma’s Shocking Secret to a Hollywood Smile: Guava Leaves Unveiled!

Mix Cloves with Vaseline: A Secret Nobody Will Ever Tell You (Thank Me Later)

The Giant Pink Rabbit of Italy: From Knitted Monument to Decaying Legacy
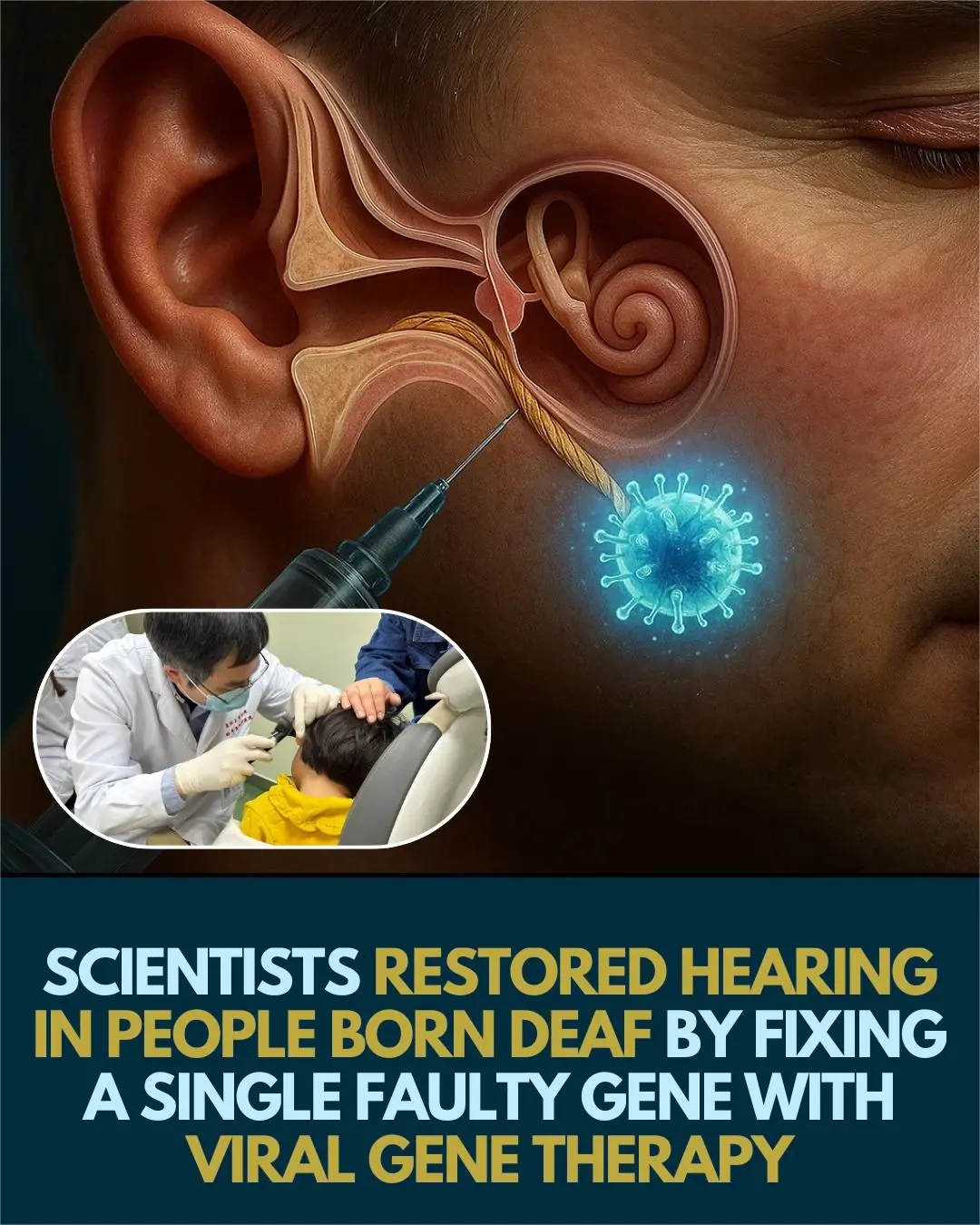
Gene Therapy Breakthrough: Restoring Hearing in Deaf Individuals via Single-Gene Repair
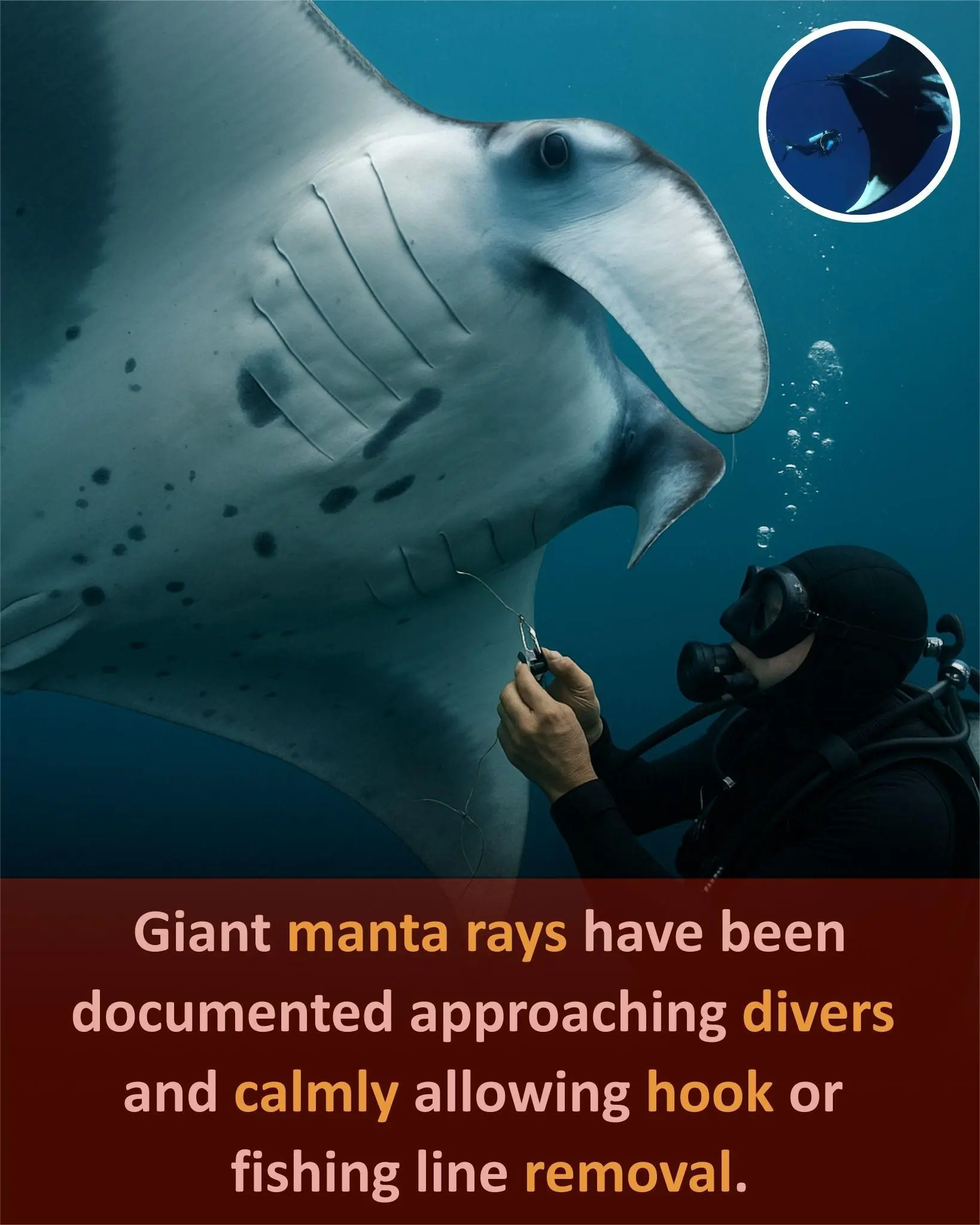
Giant Manta Ray Approaches Divers for Help in Removing Fishing Hooks

See the Difference: A Delicious Drink to Support Eye Health Naturally

Avocado, Hibiscus & Clove Smoothie: A Vibrant Blend for Energy, Digestion & Glow

Take Honey and Cloves After 50: Fix 13 Common Health Issues in One Week!

A 4-Year-Old Girl Nearly Lost Her Life Due to Diabetes, Parents Cried: “We Spoiled Her Too Much!”
