
The Hidden Problems of PCR Testing During Pandemics
The use of Polymerase Chain Reaction (PCR) testing as the gold standard for diagnosing COVID-19 was a widely accepted practice throughout the pandemic. However, numerous publications in peer-reviewed medical journals have pointed out significant flaws in how PCR tests were used to determine infectiousness. Unfortunately, this critical information was not widely disseminated to the public, creating a divide between those who understood the limitations of PCR testing and those who did not.
Misconceptions About PCR Test Positivity
A letter published in the Journal of Infection titled “The performance of the SARS-CoV-2 RT-PCR test as a tool for detecting SARS-CoV-2 infection in the population” revealed a major flaw in the way PCR tests were used:
"In light of our findings that more than half of individuals with positive PCR test results are unlikely to have been infectious, RT-PCR test positivity should not be taken as an accurate measure of infectious SARS-CoV-2 incidence."
This research confirms that a significant proportion of individuals who tested positive for COVID-19 via PCR were not actually infectious at the time of testing. Studies estimate that between 50-75% of PCR-positive cases may have been post-infectious, meaning the individual was no longer capable of spreading the virus.
How PCR Testing Works and Its Limitations
PCR tests work by amplifying genetic material from a virus. The process involves multiple cycles of amplification to detect viral RNA in a sample. The fewer cycles required to detect viral material, the higher the viral load in a person, indicating a greater likelihood of active infection. Conversely, if more cycles are needed, it suggests only trace amounts of viral material, which may not indicate an active infection.
A study published in Clinical Infectious Diseases titled “Correlation Between 3790 Quantitative Polymerase Chain Reaction–Positives Samples and Positive Cell Cultures” found that among positive PCR samples where cycle thresholds (Ct) were above 35, only 3% of samples contained replicable virus. This means that:
-
If someone tested PCR positive at a Ct of 35 or higher, the probability of them being actively infected was less than 3%.
-
The probability of that test result being a false positive (i.e., a non-infectious person testing positive) was 97%.
The Impact of High Cycle Thresholds
During the COVID-19 pandemic, high Ct values (35 or more) were commonly used, leading to an increase in positive results even among asymptomatic or non-infectious individuals. This resulted in:
-
Healthy individuals testing positive without symptoms.
-
People who had recovered from COVID-19 weeks or months earlier still testing positive, despite not being infectious.
-
Unnecessary quarantines and lockdowns based on inaccurate assessments of infectiousness.
Why Was This Issue Ignored?
Many virologists and epidemiologists attempted to bring attention to this problem, but their concerns were largely dismissed or censored. The narrative that “a positive PCR test equals an active COVID-19 case” was propagated, even though scientific evidence showed that PCR positivity alone was not a reliable measure of active infection.
Historically, similar issues with false positives and over-reliance on PCR tests have been seen in other viral outbreaks. Yet, instead of addressing these concerns, public health officials and policymakers doubled down on widespread testing without adjusting for cycle threshold limitations.
Conclusion: The Need for Transparent Testing Standards
The pandemic has highlighted the urgent need for better public understanding of PCR testing and how it should be interpreted. Moving forward, it is crucial that health authorities:
-
Clarify PCR limitations to the public and healthcare professionals.
-
Use cycle thresholds appropriately to distinguish between active and non-active infections.
-
Incorporate additional diagnostic tools like antigen tests and clinical symptoms rather than relying solely on PCR.
-
Encourage scientific discourse rather than censoring experts raising valid concerns.
The failure to properly communicate the limitations of PCR testing contributed to unnecessary fear, misdiagnoses, and misguided public health decisions. A more balanced and transparent approach is essential for handling future outbreaks effectively.
News in the same category

People Are Only Just Realizing Why Women’s Underwear Have A Bow On Front

Chroming: Social media trend of inhaling toxic chemicals to get high takes teen girl’s life

Brandi Glanville Says There's an 'Oily Foul-Tasting Drainage' from Her Face That's 'Eating Away at My Teeth'

91-Year-Old Mother Kicked Out by Her Own Son, Forced to Sleep Outside: A Heartbreaking Truth Unfolds

Realizing Something Was Off: How One Man’s Work Habits Led to a Surprising Diagnosis
Rodrigo Duterte Opposes Detention at Villamor: "I Was Brought Here Not of My Own Volition"
News Post

What Happens When You Eat Sweet Potatoes for Breakfast Every Day? The Results May Surprise You!

“Taking Medicine After a Meal Is Useless?” When Is the Best Time to Take Medication?

Eating Peanuts on an Empty Stomach Every Morning: 6 Health Benefits You Might Experience in Just 15 Days

Durian: A Nutritional Powerhouse, But Beware These 7 Risks When Eating It

Can Sleep Reveal Cancer? If You Notice These 4 Sleep Abnormalities, Get Checked ASAP

Can Your Hand Back Reveal Your Longevity? 4 Signs of a Long Life

Start Your Day with a Bowl of “Hot Water Egg” – See What Happens to Your Body After a While!

Little Girl Stopped Me on the Street and Said, 'Your Picture Is in My Mom's Wallet!' – When I Saw Her Mom, I Was Speechless
5 Reasons to Have Protein Before Bed
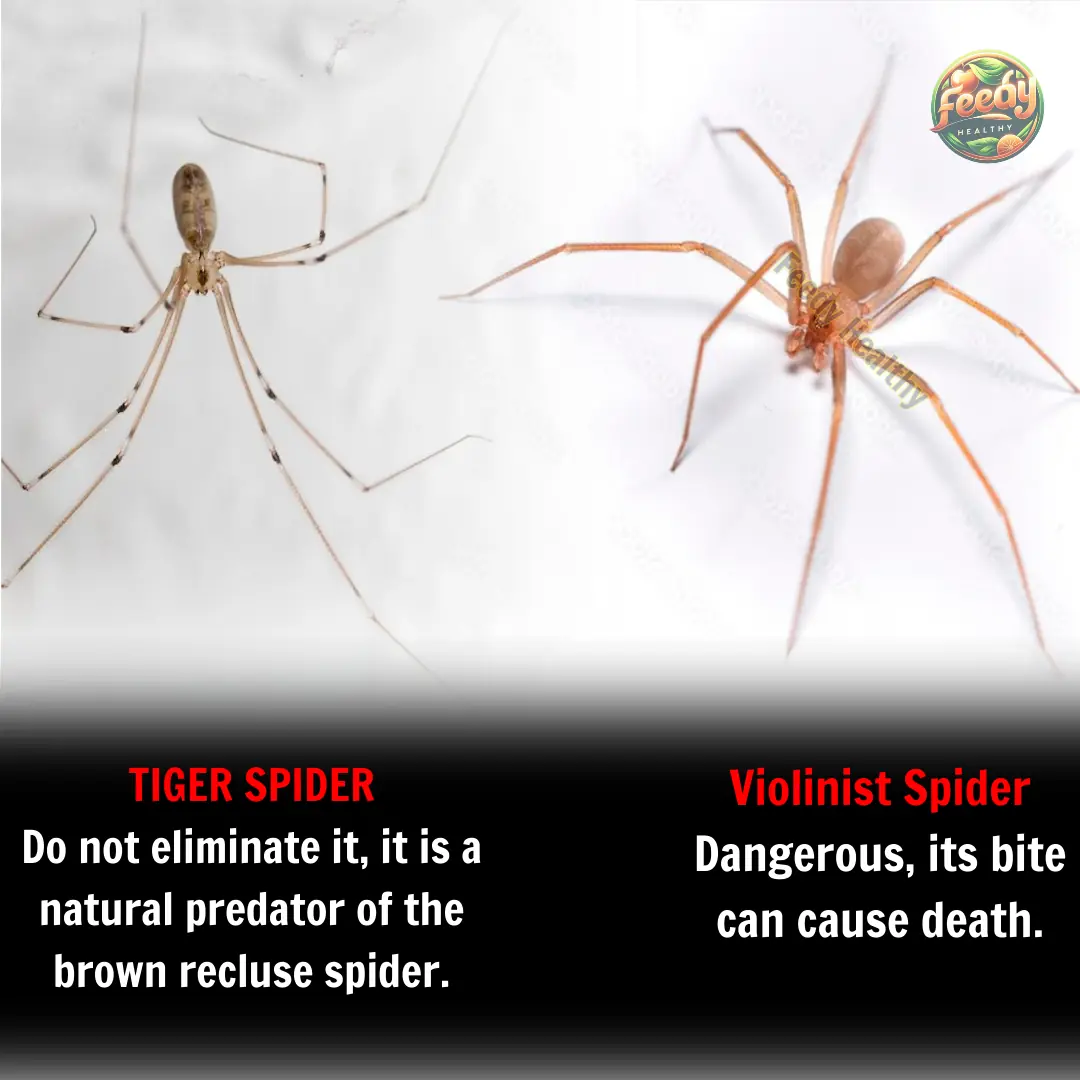
The Tiger Spider: Nature’s Defense Against the Violin Spider

Tailors don’t want you to know this secret! Fix any zipper in 2 minutes.

A Millionaire Gifted Me a House as a Mother of 5, When I Entered and Read the Note Left Inside, I Froze in Sh0ck
9 Foods to Consider Limit if You Have Hypothyroidism

Runner’s Terminal Cancer Diagnosis Sparks Urgent Warning on the Dangers of Overlooking Minor Symptom
People Are Only Just Realizing Why Women’s Underwear Have A Bow On Front

My Neighbor Kept Hanging out Her Panties Right in Front of My Son's Window – So I Taught Her a Real Lesson
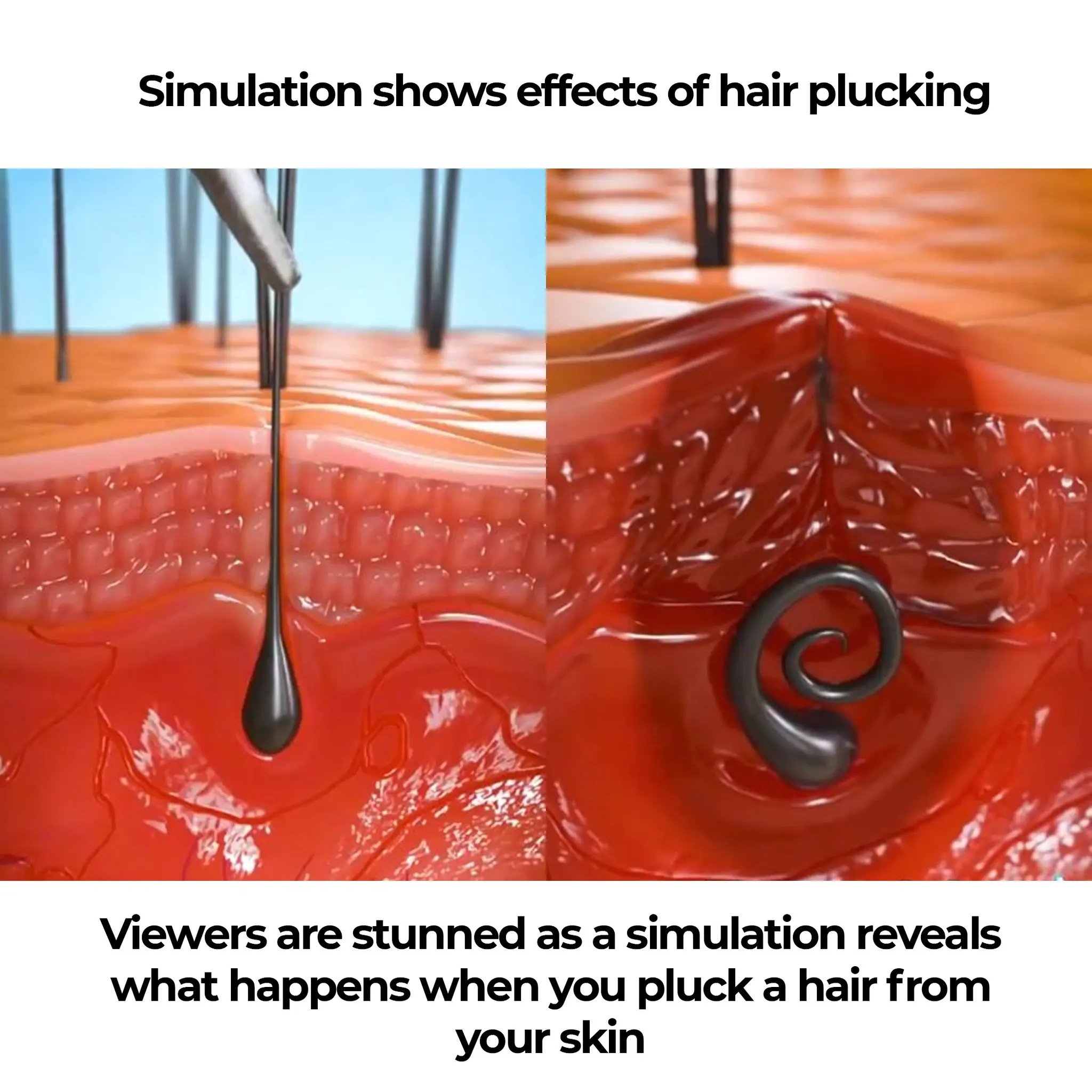
Viewers are stunned as a simulation reveals what happens when you pluck a hair from your skin

7 Exercises to Help Prevent Spider and Varicose Veins
