Study Suggests Key Link That Could Help Explain Autism Development

In recent years, scientists have increasingly uncovered just how vital our gut microbiota is to overall health. From our ability to process stress to weight regulation, mental health, and susceptibility to autoimmune diseases like type 1 diabetes and lupus — the microbes in our digestive tract play a pivotal role.
Now, a new study published in The Journal of Immunology adds to this growing body of evidence, revealing a surprising link between the maternal gut microbiome and the development of autism spectrum disorder (ASD) in offspring.
Gut-Brain Connection: A Deeper Look
Led by John Lukens, PhD, at the University of Virginia School of Medicine, the research highlights how a mother’s microbiota may exert more influence on a child’s neurological development than the child’s own microbiome.
“The microbiome is really important to the calibration of how the offspring’s immune system is going to respond to an infection or injury or stress,” said Lukens. “It can shape the developing brain in multiple ways.”
At the center of this discovery is a molecule produced by the immune system, interleukin-17a (IL-17a) — a cytokine previously associated with inflammatory diseases such as psoriasis, multiple sclerosis, and rheumatoid arthritis. IL-17a plays a vital role in protecting against infections, particularly fungal ones, but it also appears to impact fetal brain development in the womb.
The Experiment: How Gut Bacteria Shape the Brain
Using lab mice, the team explored how maternal microbiota and immune responses may influence neurodevelopment. Mice from two separate labs were selected:
-
The first group of female mice had gut bacteria that promoted an inflammatory response via IL-17a.
-
The second group served as the control and did not show the same predisposition.
Researchers artificially suppressed IL-17a in both groups during pregnancy. As a result, all offspring displayed normal (neurotypical) behavior at birth — a promising sign that suppressing inflammation might reduce autism risk.
However, when the natural IL-17a response was allowed to proceed, the pups born to the first group of mothers (those with the pro-inflammatory gut microbiota) later developed autism-like behaviors, including impaired social interaction and repetitive actions.
To confirm that gut bacteria were the driving factor, scientists transplanted fecal matter from the first group into the second group. The offspring of this now-altered second group also developed autism-like symptoms, providing strong evidence that maternal microbiota alone could trigger neurological changes in the developing brain.
What This Means — And What’s Next
While these results are based on animal models and don’t necessarily translate directly to humans, they open a powerful new avenue for autism research. The findings suggest that a mother's gut health — particularly how it shapes inflammatory immune responses during pregnancy — may influence the neurological development of her child.
“This is just the beginning,” Lukens said. “There are many more molecules to investigate. IL-17a may be just one piece of a much larger puzzle.”
The next phase of research will aim to identify which specific microbes or microbial metabolites in the maternal microbiome are responsible for influencing brain development — and whether similar patterns can be detected in humans.
A Bigger Picture: Microbiota, Inflammation, and Prevention
As understanding of the gut-brain axis deepens, this study adds urgency to the call for better maternal care — not only in terms of diet and stress management but also in microbial health. It raises important questions:
-
Can modifying the maternal microbiome reduce the risk of autism?
-
Are there safe ways to regulate immune responses during pregnancy?
-
Could probiotics or dietary changes make a measurable difference?
While definitive answers remain out of reach, one thing is clear: the microbiome is not just a digestive issue — it's a developmental one.
In Summary:
-
A mother's gut bacteria can influence her offspring’s brain development through immune signaling.
-
IL-17a, an inflammatory molecule, may play a critical role in autism-like symptoms.
-
Fecal transplant experiments confirmed the impact of maternal microbiota.
-
More research is needed to explore human implications, but the potential is profound.
As we continue to unravel the hidden dialogue between microbes and the mind, this research underscores a powerful truth: the foundations of neurological health may begin in the gut — even before birth.
News in the same category

Pope Francis’ shocking net worth at his time of death

5 Countries Making It Harder for Americans to Live and Work Abroad
Chilling last words of trainer ripped apart by ‘psychotic’ killer whales

Animal lover finds squirrel with giant tooth, brings him home and gives him a new opportunity – thank you
10 Benefits to Drinking Warm Water (No Lemon Required)

Zookeepers refuse to save drowning chimpanzee – then a truck driver breaks into his cage

College student has fatal reaction to brownie she got from friend

Why You Should (and Shouldn’t) Be Hanging Your Clothes Outside

Cabbage: A Nutrient-Packed Superfood, But Some People May Need to Avoid It

Pope Francis’ final words before passing aged 88

Tokyo Hospital Introduces New Baby Box for Abandoned Infants
A Wake-Up Call Hidden In Metal: The Colombian Sphere Mystery “Revealed”

Japan Green Traffic Lights: The Curious Case of Blue Signals

Friendship Marriages Gain Traction in Japan as Alternative to Traditional Unions
Father of bullied boy who killed himself one year ago shares tragic twist

California on Alert After Discovery of 13-foot Climbing Invasive Creature from China

5 years old saves sister, dog from burning home then alerts rest of family

Orangutan mom, thought to be infertile, gives birth and is captured on camera for the first time
News Post

Mix avocado seed with olive oil.

Natural Pest Control with Baking Soda & Vinegar

Boost Your Hair Health with Clove and Rosemary Water Hair Growth Spray

Discover the Magic of Salted Orange Peels

Enhancing Your Vision With Cucumbers

Eliminates mucus from the lungs at the root, helps soothe dry cough.

Abandoned “unicorn” puppy with tail growing from his head rescued from freezing cold

For 3 hours woman stays with trapped horse – then a farmer does everything he can to save its life
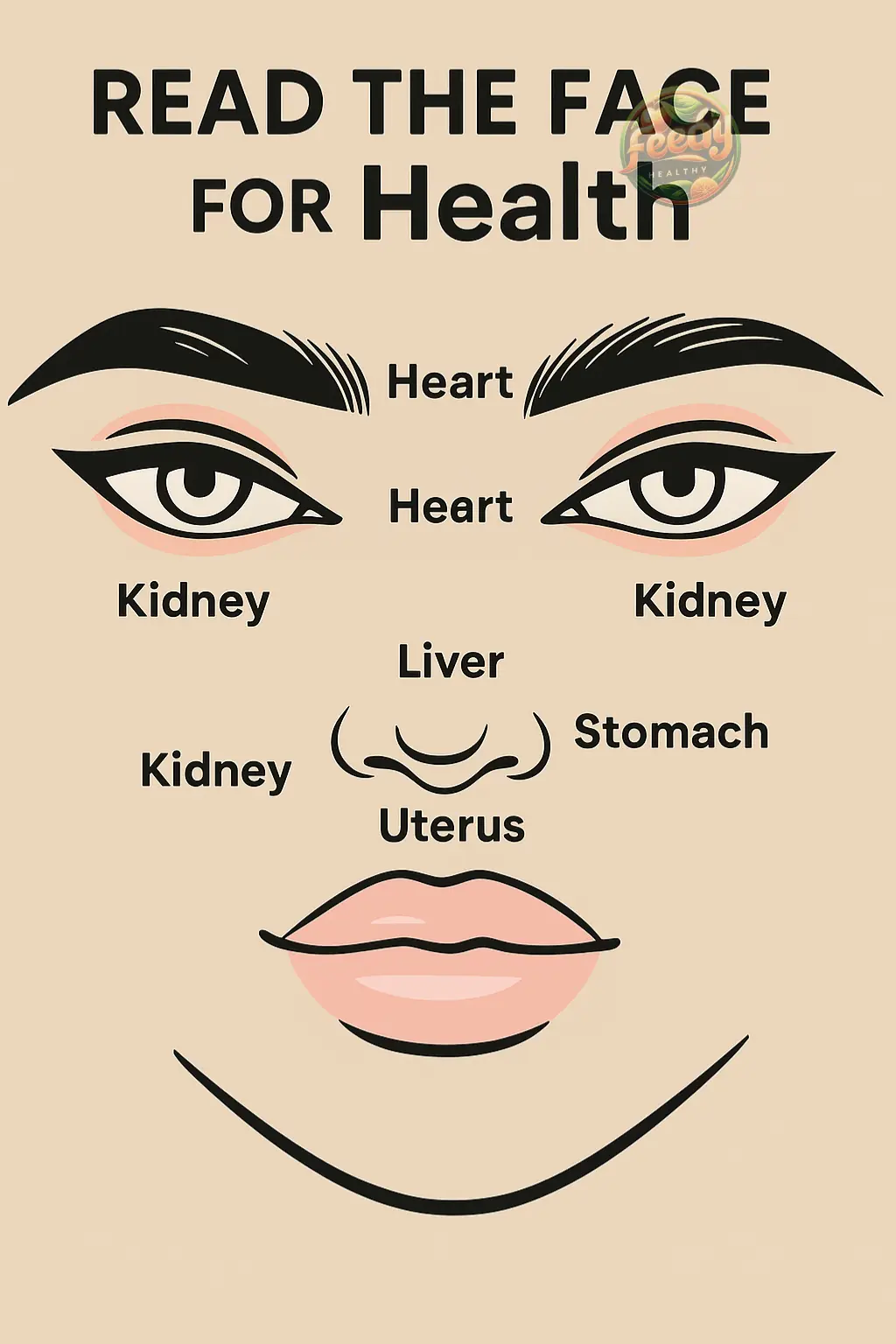
Learn to Listen to Your Body: Read the Face for Health
Korean Rice Cream: The Ageless Skincare Secret Revealed

Henna Hacks: How Cloves Unlock Darker, Richer Stains Naturally

🌿 Oregano Orejón: Improve Your Vision and Much More

The Hidden Power of Guava Leaves for Blood Sugar Control: What Every Diabetic Should Know

Unbelievable! ? Destroy Varicose Veins and Inflammation Naturally with Garlic

The plant that helps regulate blood sugar levels, supports the pancreas, and is useful for high blood pressure and Alzheimer's.

Put Lemon with Garlic and You May Never Have to Visit a Hospital Again

Varicose Veins Have Disappeared Without a Trace! No More Foot Pain – 100% Natural Remedy with Red Onion!
The Anti-Aging Carrot Drink: A Centenarian’s Daily Elixir